Screening Strategies for Hepatitis: Identifying At-Risk Populations and Implementing Effective Testing
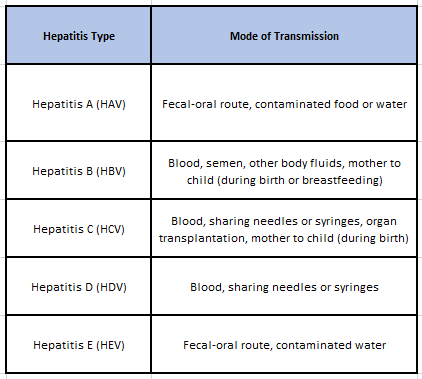
Hepatitis is a viral disease causing liver inflammation, affecting millions of people worldwide with an estimated 345 million individuals living with chronic infections.1 Hepatitis surpasses the mortality rates of HIV/AIDS, tuberculosis, and malaria combined at ~1.3 million deaths each year. Hepatitis presents with varying outcomes: self-limiting, fibrosis, cirrhosis, or liver cancer. While the five main Hepatitis viruses (A, B, C, D, and E) are the primary cause of high illness burden, interactions with other infections, toxins (e.g., alcohol, drugs), and autoimmune diseases can also contribute to the high mortality and potential for epidemics.2 Types B and C, especially, cause chronic diseases, impacting millions and being the top causes of liver cirrhosis and cancer.
The worldwide strategy for hepatitis by the World Health Organization, supported by all its member nations, seeks to decrease new hepatitis cases by 90% and fatalities by 65% from 2016 to 2030. Read this article to implement a strategy and contribute to the mitigation of hepatitis globally.
Modes of Transmission and Risk Factors
Identifying At-Risk Populations
1. Geographical Considerations
- Prevalence in Different Regions:
The prevalence of hepatitis can vary significantly between different regions and countries. Certain regions may have a higher prevalence of hepatitis due to factors such as endemicity, inadequate healthcare infrastructure, and limited access to prevention measures.
HAV is highly endemic in Africa and Asia, with a large proportion of the population immune to the virus. HBV and HCV infections are particularly burdensome in sub-Saharan Africa. The Americas have a high prevalence of hepatitis A, except for high-income North American countries, and a significant number of HBV cases imported through immigration. Eastern Mediterranean countries have seen a decrease in hepatitis A incidence, while HBV and HCV infections remain a concern. South-East Asia has high HAV seroprevalence, a significant burden of chronic viral hepatitis, and a high number of HEV infections. The Western Pacific region has a large population and a high burden of viral hepatitis, particularly HBV and HCV, contributing to a significant number of liver cancer cases.6 Understanding the prevalence rates in different regions helps in tailoring screening and prevention programs accordingly.
- Migration and Travel Patterns:
According to the UN’s World Migration Report of 2022,7 there were around 281 million international migrants in the world in 2020, which equates to 3.6 per cent of the global population then. Migration and travel patterns contribute to the spread of hepatitis infections. Individuals who migrate from regions with high hepatitis prevalence to low-prevalence areas can introduce the virus to new populations.8 Similarly, travelers visiting areas with higher hepatitis prevalence can be exposed to the virus. Identifying geographic areas with a high influx of migrants or travelers helps in implementing targeted testing and prevention strategies.
2. Socioeconomic Factors
- Poverty and Lack of Access to Healthcare:
Socioeconomic factors, such as poverty and limited access to healthcare, play a significant role in the risk of hepatitis transmission.9 People living in poverty often face barriers to healthcare services, including vaccinations, screening tests, and access to appropriate treatment. Lack of financial resources and healthcare coverage can prevent individuals from seeking timely medical care, increasing the likelihood of transmission within these populations.
- Incarceration Rates and Risk of Transmission:
Incarcerated individuals are considered a high-risk population for hepatitis due to various factors. Overcrowding, limited access to preventive measures, and a higher prevalence of injection drug use within correctional facilities contribute to the risk of hepatitis transmission.10 Additionally, individuals who have a history of incarceration may continue engaging in high-risk behaviors even after release, further contributing to the spread of hepatitis in the community.
3. High-Risk Conditions
- Explosure due to Infected Patients:
According to a study conducted to evaluate risk of occupational exposure to blood-borne viruses and determine the prevalence of human immunodeficiency virus (HIV), hepatitis B virus (HBV) and hepatitis C virus (HCV) among HCWs in Georgia, it was found that out of 1386 participating healthcare workers, the prevalence of HCV infection was among 5%, while 29% showed anti-HBc with 2% being HBsAg carriers.5 Accidental needlestick injuries, improper handling of contaminated equipment, and exposure to infected patients can lead to these transmissions. Healthcare settings pose a higher risk due to the higher concentration of infected individuals seeking medical care.
- Unsafe Needle and Drug Paraphernalia Usage:
Injection drug users (IDUs) are considered a high-risk population for hepatitis due to the sharing of needles and other drug paraphernalia. Hepatitis B and C viruses can be transmitted through contaminated blood and bodily fluids present on shared injection equipment.1 The close proximity and frequent sharing of needles among IDUs create an environment conducive to viral transmission.
- Unsafe Sexual Practices:
Men who have sex with men (MSM) and individuals with multiples sexual partners are another population at an increased risk of hepatitis. Risky sexual behaviors, such as unprotected intercourse, can lead to the increased transmission of hepatitis viruses.3, 4 Hepatitis A, B, and C can be transmitted through sexual contact, especially when there are open sores or mucosal tears present.
Types of Hepatitis Screening Tests
Serological Tests:
Hepatitis blood tests are designed to identify antigens or antibodies that are specific to each type of hepatitis virus.11 They can identify both past and current infections and determine the specific type of hepatitis virus present.
Nucleic Acid Tests:
Nucleic acid tests are highly sensitive and specific, allowing for early detection of viral infections, even before antibodies are produced.11 Nucleic acid tests are particularly useful in high-risk populations, immunocompromised individuals, and in monitoring treatment response.
Optimal Timing for Screening
-
One-Time Screening vs. Periodic Testing:
One-time screening involves testing individuals for hepatitis infection at a specific point in time.12 This approach is commonly used in high-risk populations, such as individuals with known risk factors or those seeking healthcare services. Periodic testing, on the other hand, involves regular screening at recommended intervals, especially in populations with ongoing risk exposures. The optimal timing for periodic testing depends on the specific risk factors and guidelines provided by healthcare authorities.
-
Screening Pregnant Women and Newborns:
Screening pregnant women for hepatitis B is a critical strategy to prevent mother-to-child transmission. It allows for timely administration of preventive interventions, such as antiviral medications and hepatitis B vaccination for newborns. Newborns of mothers who test positive for hepatitis B should receive post-exposure prophylaxis to reduce the risk of transmission.
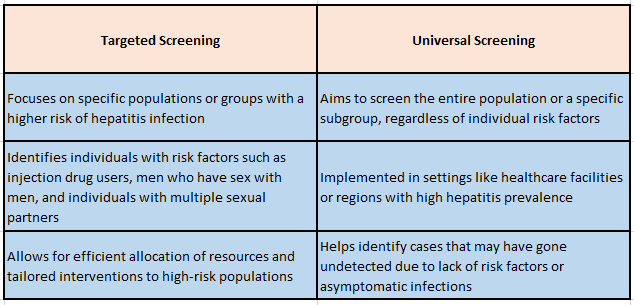
Targeted vs. Universal Screening Approaches
Strategies for Implementing Effective Hepatitis Testing
1. Education and Awareness Campaigns
Education and awareness campaigns play a vital role in implementing effective testing strategies for hepatitis. These campaigns aim to:
Increase Knowledge: Education campaigns provide information about hepatitis, its modes of transmission, risk factors, and the importance of testing.1 They help individuals understand the significance of early detection, treatment options, and preventive measures.
Reduce Stigma: Stigma surrounding hepatitis infections can discourage individuals from seeking testing. Awareness campaigns help combat stigma by promoting understanding, empathy, and non-discrimination towards individuals living with hepatitis.
Promote Testing Services: Education campaigns raise awareness about the availability of testing services, their benefits, and the locations where testing can be accessed.1 They provide information on how and where individuals can get tested, including community clinics, healthcare facilities, or specialized testing centers.
2. Improving Accessibility to Testing Services
To implement effective testing strategies, it is crucial to improve accessibility to testing services. This can be achieved through:
Outreach Programs: Outreach programs aim to bring testing services closer to at-risk populations, particularly those who face barriers to accessing healthcare.13 Mobile testing units, community-based testing initiatives, and partnerships with community organizations can help reach individuals who may not typically seek medical care.
Targeted Testing Campaigns: Tailored testing campaigns focus on specific at-risk populations or regions with higher prevalence rates. These campaigns employ targeted messaging, culturally appropriate materials, and community engagement to encourage individuals to get tested.
Integration with Existing Healthcare Services: Integrating hepatitis testing into existing healthcare services, such as primary care or sexually transmitted infection clinics, ensures that individuals have access to testing during routine medical visits.14 This integration streamlines the process, making it more convenient and efficient for individuals to get tested.
3. Collaboration With Healthcare Providers and Community Organizations
Collaboration between healthcare providers, community organizations, and public health authorities is essential for effective testing implementation. This collaboration can involve:
Training and Capacity Building: Healthcare providers should receive training on hepatitis screening guidelines, testing protocols, and risk assessment to ensure accurate and standardized testing practices.5 Collaboration with community organizations can help provide training and resources to healthcare providers and support community-based testing initiatives.
Referral Systems: Establishing effective referral systems between testing sites and healthcare providers ensures that individuals with positive test results are connected to appropriate care and follow-up services.13 Collaboration between testing sites and healthcare providers enables seamless coordination of care and treatment.
Data Sharing and Surveillance: Collaboration between stakeholders facilitates data sharing, which is critical for monitoring and evaluating the impact of testing strategies. Sharing anonymized testing data with public health authorities can help improve surveillance, inform policies, and guide resource allocation.15
4. Integration of Testing into Routine Healthcare Visits
Integrating hepatitis testing into routine healthcare visits ensures that testing becomes a standard part of healthcare services. This integration can involve:
Healthcare Provider Education: Healthcare providers should be educated about the importance of hepatitis testing and be knowledgeable about screening guidelines. Training providers on risk assessment, testing methods, and interpretation of test results promotes consistent and systematic testing practices.1
Routine Screening Protocols: Implementing routine screening protocols ensures that healthcare providers routinely offer hepatitis testing to individuals based on established guidelines.1 Incorporating reminders and prompts in electronic medical records can help healthcare providers adhere to testing protocols.
By implementing these strategies, healthcare systems and organizations can effectively conduct hepatitis testing programs, increase awareness and testing rates, and ensure appropriate care and treatment for individuals diagnosed with hepatitis. It is also important to regularly assess screening coverage, monitor disease trends, track program outcomes, and conduct cost-effectiveness analysis, healthcare authorities to refine screening strategies and ensure the best possible outcomes for individuals affected by hepatitis.
References:
- 2019. “Hepatitis.” www.who.int. September 1, 2019. https://www.who.int/news-room/questions-and-answers/item/hepatitis.
- Jefferies, Meryem, Bisma Rauff, Harunor Rashid, Thao Lam, and Shafquat Rafiq. 2018. “Update on Global Epidemiology of Viral Hepatitis and Preventive Strategies.” World Journal of Clinical Cases6 (13): 589–99. https://doi.org/10.12998/wjcc.v6.i13.589.
- Turner, J M. 2006. “Behavioural Predictors of Subsequent Hepatitis c Diagnosis in a UK Clinic Sample of HIV Positive Men Who Have Sex with Men.” Sexually Transmitted Infections82 (4): 298–300. https://doi.org/10.1136/sti.2005.018366.
- “Sexual Transmission and Viral Hepatitis | CDC.” 2021. www.cdc.gov. April 22, 2021. https://www.cdc.gov/hepatitis/populations/stds.htm#:~:text=Sexual%20Transmission%20and%20Hepatitis%20B.
- Butsashvili, M., G. Kamkamidze, M. Kajaia, D. L. Morse, W. Triner, J. DeHovitz, and L.- A. McNutt. 2012. “Occupational Exposure to Body Fluids among Health Care Workers in Georgia.” Occupational Medicine62 (8): 620–26. https://doi.org/10.1093/occmed/kqs121.
- Jefferies, Meryem, Bisma Rauff, Harunor Rashid, Thao Lam, and Shafquat Rafiq. 2018. “Update on Global Epidemiology of Viral Hepatitis and Preventive Strategies.” World Journal of Clinical Cases6 (13): 589–99. https://doi.org/10.12998/wjcc.v6.i13.589.
- INTERNATIONAL ORGANIZATION FOR MIGRATION. 2022. “World Migration Report 2022.” Iom.int. 2022. https://worldmigrationreport.iom.int/wmr-2022-interactive/.
- Sharma, Suraj, Manuel Carballo, Jordan J. Feld, and Harry L.A. Janssen. 2015. “Immigration and Viral Hepatitis.” Journal of Hepatology63 (2): 515–22. https://doi.org/10.1016/j.jhep.2015.04.026.
- Tulane University. 2021. “Social Determinant of Health: Education Is Crucial.” Publichealth.tulane.edu. January 27, 2021. https://publichealth.tulane.edu/blog/social-determinant-of-health-education-is-crucial/.
- Belaunzarán-Zamudio, Pablo F., Juan L. Mosqueda-Gomez, Alejando Macias-Hernandez, Juan G. Sierra-Madero, Saifuddin Ahmed, and Chris Beyrer. 2017. “Risk Factors for Prevalent Hepatitis c Virus-Infection among Inmates in a State Prison System in Mexico.” Edited by Viviane D. Lima. PLOS ONE12 (6): e0179931. https://doi.org/10.1371/journal.pone.0179931.
- Center for Substance Abuse Treatment. 2011. “Screening for Viral Hepatitis.” Nih.gov. Substance Abuse and Mental Health Services Administration (US). 2011. https://www.ncbi.nlm.nih.gov/books/NBK92029/.
- 2020. “Testing Recommendations for Hepatitis c Virus Infection | HCV | Division of Viral Hepatitis | CDC.” Www.cdc.gov. March 9, 2020. https://www.cdc.gov/hepatitis/hcv/guidelinesc.htm.
- “Chapter 5: Outreach Programs: Planning, Implementation and Evaluation – Lets Yarn.” n.d. Letsyarn.health.wa.gov.au. https://letsyarn.health.wa.gov.au/tttt/chapter-5.
- “Public Health Guidance on HIV, Hepatitis B and c Testing in the EU/EEA an Integrated Approach.” n.d. https://www.ecdc.europa.eu/sites/default/files/documents/hiv-hep-testing-guidance_0.pdf.
- Groseclose, Samuel L., and David L. Buckeridge. 2017. “Public Health Surveillance Systems: Recent Advances in Their Use and Evaluation.” Annual Review of Public Health38 (1): 57–79. https://doi.org/10.1146/annurev-publhealth-031816-044348.
Author:

Uttkarsha Bhosale
Editor, Enago Academy
Medical Writer, Enago Life Sciences
Connect with Uttkarsha on LinkedIn