The growing dominance of digital platforms in healthcare communication introduces a persistent challenge: how can we ensure equitable access in low-resource settings? While high-income countries are rapidly adopting telehealth, AI-powered documentation, and virtual medical conferences, large parts of the world continue to face a “digital divide”, posing a public health and equity challenge. Poorly designed communication strategies risk excluding the very populations that most need timely, accurate, and culturally appropriate health information.
Bridging this divide requires more than simply deploying technology. It demands infrastructure investment, digital literacy education, community partnerships, and policy reforms that prioritize equity and local context.
Key Barriers in Low-Resource Settings
Medical communication in low-resource environments is shaped by interconnected challenges rather than isolated obstacles. In a global study, 21% of healthcare providers reported poor access to interpreter services, and 37% felt patients withheld information due to language barriers. Three key barriers stand out:
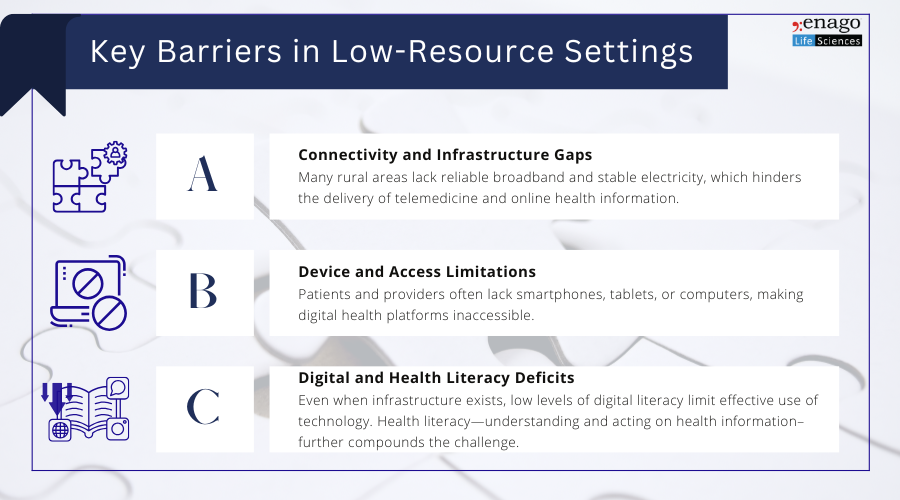
While these barriers create significant hurdles, they also reveal clear areas for intervention. By targeting infrastructure, device availability, and digital literacy simultaneously, stakeholders can design practical strategies that not only bridge the divide but also make medical communication more inclusive and sustainable in low-resource settings.
Practical Strategies for Bridging the Divide
1. Expand Broadband and Device Access
Governments, NGOs, and private partners should prioritize:
- Expanding rural broadband through satellite and mobile internet projects.
- Subsidized or loaner devices to patients and community health centers, to ensure equitable participation in digital health programs.
2. Promote Digital Literacy
Education must target both patients and providers:
- Community-based training programs to build confidence in using apps, telehealth platforms, and online portals.
- Peer and family support networks to encourage adoption particularly among elderly or rural populations.
3. Use Mobile Health and Telemedicine
Design technology that works in constrained environments:
- Mobile-first applications optimized for low bandwidth.
- Telemedicine platforms tailored for low-literacy users, with voice and language support.
4. Invest in Community Health Centers as Digital Hubs
Local health facilities can serve as digital access points where:
- Patients receive assistance with telehealth visits, medication management, and preventive care.
- Providers are receiving training in digital tools and supported with IT resources.
5. Reduce Financial Barriers
Affordability is critical for sustainability:
- Public-private partnerships to subsidize connectivity.
- Insurance coverage and policy support to offset costs of telehealth and e-health services.
6. Contextualize Technology Solutions
Cultural, linguistic, and socioeconomic factors must guide implementation. Locally adapted solutions—such as multilingual interfaces, offline features, or culturally relevant health messaging—are far more likely to succeed.
Without deliberate action, disparities in digital access risk compounding existing inequities in health outcomes. The evidence is clear: when infrastructure, digital literacy, and inclusive policies align, even the most resource-constrained settings can leverage technology to transform patient care.
At Enago Life Sciences, we are committed to advancing equitable medical communication by supporting researchers, healthcare professionals, and organizations in developing strategies that resonate across diverse settings. Together, we can ensure that the future of health communication is inclusive, patient-centered, and universally accessible.
Author:

Anagha Nair
Editorial Assistant, Enago Academy
Medical Writer, Enago Life Sciences
Connect with Anagha on LinkedIn
