Key Takeaways
Interprofessional Education (IPE) is a transformative approach to healthcare education that prepares students from diverse disciplines—such as medicine, nursing, pharmacy, and allied health—to work collaboratively. It fosters teamwork, communication, and mutual respect, critical components for improving patient care and outcomes.
-
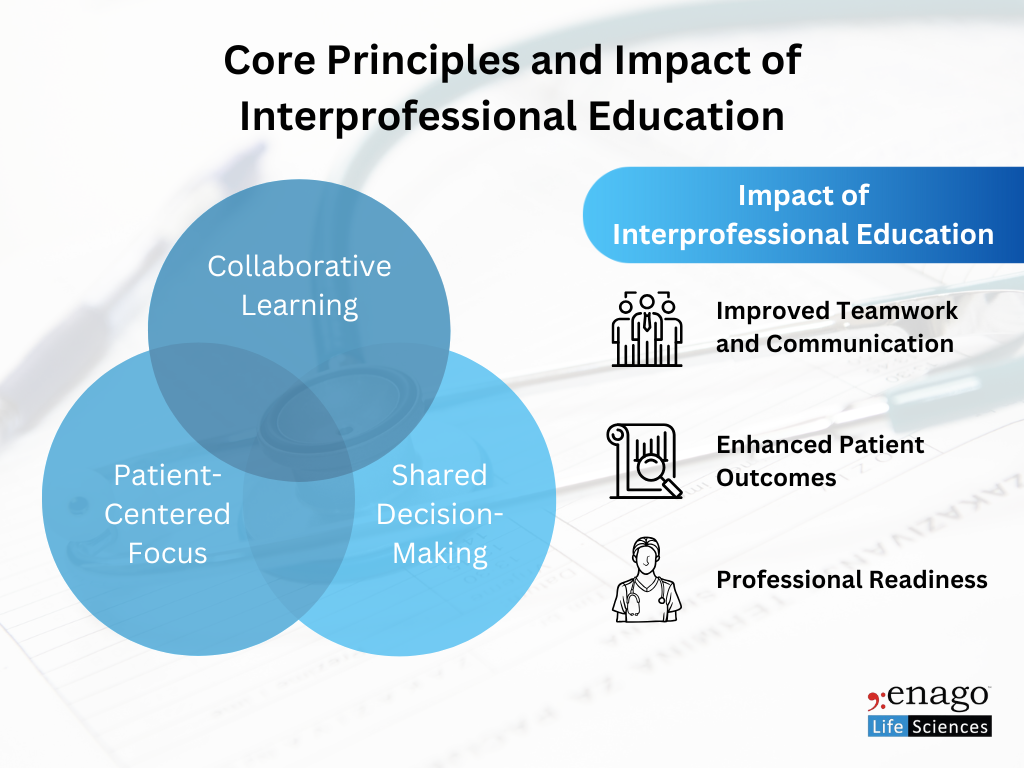
Collaborative Learning
IPE brings together students from diverse healthcare professions to learn from, with, and about each other, fostering mutual respect, shared values, and understanding of each profession’s roles and contributions.
-
Patient-Centered Focus
The primary goal of IPE is to enhance patient care by promoting effective collaboration among healthcare providers. This leads to more coordinated, responsive, and comprehensive care, especially in complex or chronic cases.
-
Shared Decision-Making
IPE encourages joint problem-solving and shared planning. It integrates the unique expertise of each discipline into care strategies, improving both the quality and safety of clinical decisions.
Impact and Outcomes
-
Improved Teamwork and Communication
IPE fosters clear role understanding, effective handovers, and mutual accountability—key factors in reducing clinical errors and improving communication.
-
Enhanced Patient Outcomes
Collaborative care models have been associated with fewer hospital readmissions, improved chronic disease management, and higher patient satisfaction.
-
Professional Readiness
Graduates trained in IPE environments demonstrate greater adaptability, teamwork, and confidence in interdisciplinary settings—skills essential for modern healthcare systems.
Key Strategies for Effective Implementation
1. Integrated Curriculum Design
- Embed IPE activities throughout the curriculum—from foundational courses to clinical placements—to support progressive competency development.
- Use instructional methods such as case-based learning, problem-based learning, simulation exercises, and collaborative projects to encourage experiential learning.
- Align learning outcomes with national and institutional competency frameworks.
2. Faculty Development and Engagement
- Provide training in interprofessional facilitation, bias mitigation, and collaborative assessment.
- Encourage co-teaching models with faculty from multiple disciplines, helping students see real examples of collaborative practice.
- Recognize and reward faculty involvement in IPE through academic credit or promotion pathways.
3. Simulation and Real-World Practice
- Use simulation platforms and standardized patient encounters to allow learners to practice teamwork and communication in safe, controlled environments.
- Engage students in real-world interprofessional scenarios like ward rounds, code blue simulations, and community-based placements to foster collaborative clinical reasoning.
4. Assessment and Continuous Improvement
- Apply validated tools such as the Interprofessional Collaborative Competency Attainment Survey (ICCAS), peer evaluations, reflective journals, and Objective Structured Clinical Examinations (OSCEs) to measure competencies.
- Implement structured feedback mechanisms to track outcomes and adapt the program based on data.
5. Alignment with Accreditation and Policy
- Ensure IPE activities align with the standards of accreditation bodies (e.g., LCME, ACPE, WHO) and institutional strategic goals.
- Advocate for dedicated funding, policy support, and formal recognition of IPE within educational governance.
Challenges and Practical Solutions
IPE offers immense benefits, but its implementation is often hindered by several systemic and cultural challenges. These include:
Challenge |
Strategy/Solution |
| Institutional silos and resistance | Secure leadership support and embed IPE into strategic plans and policies |
| Scheduling difficulties across programs | Use centralized coordination to align academic calendars and clinical rotations |
| Limited shared physical space or simulation labs | Plan joint sessions in neutral or shared spaces; invest in scalable digital simulations |
| Appoint IPE champions; offer teaching credits and professional development | |
| Curricular rigidity | Integrate IPE into core learning outcomes and leverage existing course structures |
| Cultural silos and profession-centric bias | Use role-clarification activities and diverse team-based simulations to reduce bias |
| Lack of validated assessment tools | Adopt mixed-method evaluations, reflective journals, and peer reviews |
Source: Adapted from Shakhman et al., 2020 (PMC7430136)
Institutional and Faculty-Level Strategies
To address these barriers, successful IPE programs have implemented the following:
- Leadership Commitment: IPE should be explicitly included in institutional vision, supported by a dedicated office or steering committee.
- Policy and Governance Integration: Embed IPE competencies into program outcomes and accreditation documents.
- Faculty Training and Incentives: Provide IPE facilitation workshops and incentivize participation through academic promotions or workload adjustments.
- Collaborative Curriculum Planning: Form cross-disciplinary teams to co-design content and coordinate delivery.
- Continuous Review and Research: Regularly assess IPE effectiveness and publish findings to inform best practices and support sustainability.
In today’s complex healthcare landscape, Interprofessional Education is no longer optional—it is essential. By training healthcare professionals to communicate and collaborate across boundaries, IPE leads to safer care, better patient outcomes, and stronger clinical teams. Effective implementation demands a deliberate, well-supported strategy: integrated curricula, empowered faculty, realistic practice opportunities, rigorous assessment, and alignment with policy. Institutions that embrace IPE not only enhance education but also shape the future of collaborative, patient-centered care.
References:
-
Haruta, Junji, Sayaka Sadohara, Kana Taketomi, Kiyoshi Shikino, Kazuya Nagasaki, Yuji Nishizaki, Daisuke Son, et al. 2024. “Competency Frameworks for Interprofessional Collaboration: A Scoping Review.” Journal of Interprofessional Education & Practice 39 (May): 100602. https://doi.org/10.1016/j.xjep.2024.100602
-
Riesen, Elena, Stefan Morley, Carole Clive, and Paul F. Légaré. 2021. “Interprofessional Education: A Review of Context, Learning and the Research Agenda.” Journal of Interprofessional Care 35 (1): 44–49. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7873741/.
-
Bigdeli, Shoaleh, Shabnam Shahhosseini, Nahid Dehghan Nayeri, and Abbas Ebadi. 2024. “Experiences of Nursing Students in Interprofessional Education: A Qualitative Meta-Synthesis.” American Journal of Obstetrics and Gynecology (April). https://doi.org/10.1016/j.ajog.2024.04.028
-
Xyrichis, Andreas, and Jill Reeves. 2020. “Piloting a Competency Framework for Interprofessional Education in Primary Care: A Multi-Method Study.” Human Resources for Health 18 (1): 13. https://human-resources-health.biomedcentral.com/articles/10.1186/s12960-020-00551-2.
-
Lutfiyya, May Nawal, Peggy A. Brandt, and Michael F. Cerra. 2021. “Reflections on Interprofessional Education for the Future Health Workforce.” Journal of Interprofessional Care 35 (2): 147–49. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7882276/.
Author:

Rebecca D’souza, PhD.
Associate Content Expert, Enago Academy
Connect with Rebecca on LinkedIn

