Effective communication is a cornerstone of public health, shaping the delivery of healthcare services, the success of public health campaigns, and the equitable treatment of diverse populations. In today’s interconnected and multicultural world, culturally informed communication has become essential for addressing health disparities and achieving better health outcomes. This article explores why culturally informed communication matters, highlights strategies for its implementation. It underscores its transformative potential in public health.
Cultural competency in healthcare involves developing the awareness, knowledge, and skills needed to respect and align with patients’ diverse cultural beliefs, values, and practices. This fosters better patient engagement, trust, and outcomes while addressing racial and ethnic disparities. Integrating cultural understanding into primary care strategies can bridge gaps in care, promote inclusivity, and improve healthcare accessibility.
Key Components of Cultural Competence
- Culturally informed communication refers to tailoring health messages and interactions to respect and align with diverse communities’ cultural norms, values, beliefs, and practices.
- Cultural humility involves openness, respect, and adaptability, enabling healthcare providers to learn from patients’ cultural identities while reflecting on their own biases. This practice enhances patient engagement and trust.
- Social factors such as income, education, housing, and access to care significantly impact health outcomes. Nurses and healthcare providers can integrate Social Determinants of Health (SDH) into their practice by conducting holistic assessments that consider patients’ social contexts and identify challenges like food insecurity or unstable housing.
- Patient-Centered Care (PCC) focuses on putting patients at the center of their healthcare decisions, respecting their unique needs and preferences. It emphasizes shared decision-making, where providers consider cultural norms regarding autonomy or family involvement in care. This approach enhances patient satisfaction and promotes better health outcomes.
Barriers to Effective Culturally Informed Communication
- Language Barriers: Communication challenges arise when patients and providers do not share the same language, leading to potential misunderstandings.
- Cultural Differences: Diverse cultural attitudes toward health, illness, and treatment, including reliance on traditional healing or distrust of medical interventions, can hinder effective communication.
- Time Constraints: Limited time during patient interactions reduces meaningful, culturally sensitive communication opportunities.
Key Strategies for Culturally Informed Communication
Implementing culturally informed communication in public health requires a multifaceted approach that addresses the unique needs of diverse populations. Some key recommendations for culturally competent communication include adopting family-centered care, encouraging patient feedback, leveraging community leaders, employing digital tools thoughtfully, incorporating visual aids, using professional interpreters, and providing cultural competence training to enhance understanding and inclusivity. Listed below are some strategies that can be implemented:
- Understand the Cultural Background: Conduct thorough research to understand the cultural backgrounds, values, beliefs, and health-related behaviors of the target population. Engage community leaders and stakeholders to gain insights and co-develop health initiatives.
- Use Clear and Inclusive Language: Avoid jargon and medical terminology that may be unfamiliar. Translate materials into the target audience’s preferred languages, ensuring that translations capture the cultural context.
- Support Self-Management: Align self-management approaches with patients’ cultural beliefs to empower them to actively manage their health in respectful and meaningful ways.
- Facilitate Shared Decision-Making: Respect cultural norms in decision-making, whether prioritizing family involvement or individual autonomy, to enhance satisfaction and outcomes.
- Collaborate with Social Workers: Address non-medical factors by connecting patients with resources like financial aid, housing assistance, or community programs.
- Create Tailored Care Plans: Customize care plans to address patients’ unique social challenges, ensuring practical and supportive interventions.
- Build Community Partnerships: Partner with local organizations to extend care beyond clinical settings and meet broader social needs.
- Incorporate Cultural Sensitivity Training: Equip public health professionals with training to recognize and respect cultural differences. This includes understanding non-verbal communication styles, religious practices, and traditional health beliefs.
- Collaborate with Community Leaders: Community leaders serve as trusted voices and cultural mediators. Partnering with them can amplify the reach and impact of public health messages.
- Leverage Diverse Media Channels: Use culturally relevant media, including ethnic radio stations, social media platforms, and community newspapers, to disseminate health information effectively.
- Collect Feedback and Adapt: Continuously gather feedback from the target community to evaluate the effectiveness of communication efforts. Adapt strategies to address emerging needs and preferences.
- Promote Cultural Representation: Include representatives from diverse communities in the design and execution of health campaigns to ensure authenticity and cultural relevance.
- Use of Interpreters: Using interpreters to help overcome language barriers allows patients to understand their care.
- Application of Visual Aids: In understanding the care and different options for treatment, visual aids such as pictures and diagrams could be used.
Examples of Culturally Informed Communication in Action
Several public health initiatives demonstrate the power of culturally informed communication:
- COVID-19 Vaccination Campaigns: Teams have successfully increased vaccine uptake by engaging local faith leaders, translating materials into multiple languages, and addressing vaccine hesitancy through culturally tailored messaging.
- HIV Prevention Programs: Community-based interventions in sub-Saharan Africa have incorporated traditional storytelling and local languages to educate communities about HIV prevention and treatment.
- Maternal Health Outreach: In the United States, programs targeting Black and Hispanic women have used culturally relevant doulas and midwives to improve respectful care.
Recent Developments in Culturally Informed Communication
- Addressing Vaccine Equity: The WHO has recently emphasized culturally tailored communication in their Immunization Agenda 2030 (IA2030), recognizing its importance in reducing vaccine inequities.
- Mental Health Campaigns: Several countries are rolling out culturally sensitive mental health initiatives to support refugee and immigrant populations. Emerging technologies, such as AI-driven chatbots and telehealth platforms, are now designed with cultural sensitivity features, enabling more inclusive virtual care.
The Role of Strategic Services in Culturally Informed Public Health Communication
Achieving culturally informed communication in public health requires a strategic blend of expertise, planning, and tailored solutions. Key services, such as language support, culturally appropriate care plans, and cultural competency training for staff, are essential in meeting the diverse needs of patients. These services contribute to achieving Universal Health Coverage (UHC) by 2030, improving health outcomes for underserved populations.
Health professionals can bridge cultural gaps, ensuring that public health campaigns, clinical information, and educational materials are effectively understood and trusted by various communities with the support of several service providers. For example, medical communicators, who are integral to the successful culturally competent communication in health care. They are responsible for tailoring health messages to align with the cultural norms, values, and beliefs of specific populations. They ensure that health content is not only accurate but also accessible and relatable, considering cultural differences in health perceptions and behaviors.
Medical communicators can also address language barriers with the help of translation services. They are pivotal in crafting inclusive messaging that builds trust and encourages positive health behaviors across diverse communities. Furthermore, translators ensure that health materials are accurately conveyed in different languages, maintaining the scientific integrity of the message while adapting it to suit the cultural context. Beyond literal translation, they also focus on linguistic nuances, idiomatic expressions, and culturally specific concepts to ensure that the target audience fully understands the information
Similarly, Graphic Designers amplify the impact of culturally sensitive communication by creating visually engaging materials that reflect the target population’s cultural identity. They consider cultural preferences in color, symbolism, and imagery to design visuals that are both appropriate and compelling. Whether through infographics, posters, or digital media, graphic designers ensure that the visual representation of health information is culturally relevant, enhancing comprehension and retention.
Together, these professionals form a collaborative team that ensures public health communications are not only scientifically sound but also culturally respectful, inclusive, and effective in promoting better health outcomes for diverse populations. Through their work, they help bridge cultural divides, ensuring that health messages are understood, trusted, and acted upon by all communities.
Final words
Minority populations often face worse health outcomes and higher rates of chronic diseases due to language barriers, cultural differences, and limited cultural competence in healthcare. Addressing these disparities requires culturally sensitive care that respects diverse values and experiences. Building trust with patients fosters open communication, and therefore leads to accurate diagnoses, effective treatments, and greater satisfaction. Engaging patients in healthcare decisions ensures treatments align with their values, while providing adequate time for reflection supports patient autonomy.
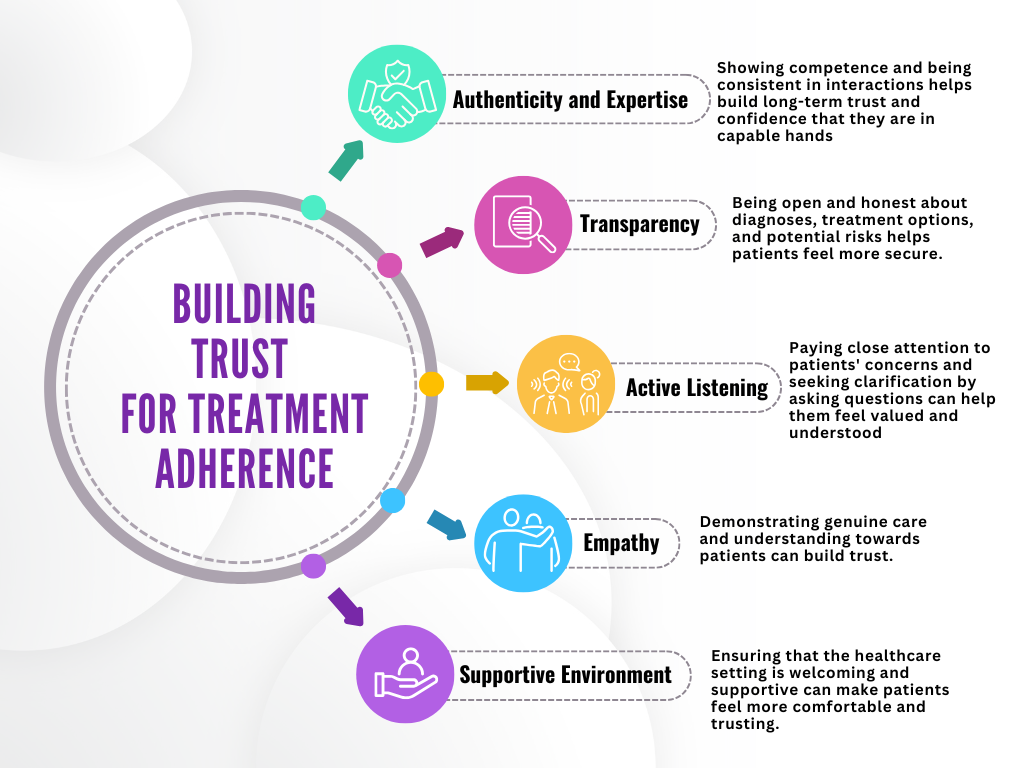
Building trust for treatment adherence involves authenticity, transparency, active listening, empathy, and a supportive environment. Thus, these elements foster patient confidence, understanding, and comfort, promoting better communication and long-term adherence to treatment plans.
Public health organizations and policymakers must invest in cultural competency training, community engagement, and interdisciplinary collaboration to address racial and ethnic disparities in healthcare.
Culturally informed communication is essential for effective public health initiatives. By integrating cultural competence into healthcare strategies, addressing barriers, and using tailored services, public health professionals can bridge disparities, enhance engagement, and improve health outcomes. Therefore, this approach is vital in creating an equitable, inclusive healthcare system for all.
References:
- Banerjee, Preetika, Rajeev Seth, Baldeep K. Dhaliwal, Alexis Sullivan, Yawar Qiayum, Betty Thankachen, Svea Closser, and Anita Shet. “Vaccine acceptance in rural India: Engaging faith leaders as vaccine ambassadors.” Frontiers in Public Health10 (2022): 979424.
- Feinberg, Iris Z., Ashli Owen-Smith, Mary Helen O’Connor, Michelle M. Ogrodnick, Richard Rothenberg, and Michael P. Eriksen. “Strengthening culturally competent health communication.” Health security19, no. S1 (2021): S-41.
- Hood, Sula, Brittany Campbell, and Katie Baker. “Culturally informed community engagement: implications for inclusive science and health equity.” (2023).
- Mallick, Lindsay M., Marie E. Thoma, and Edmond D. Shenassa. “The role of doulas in respectful care for communities of color and Medicaid recipients.” Birth49, no. 4 (2022): 823-832.
- O’Brien, Katherine L., Ephrem Lemango, Robin Nandy, and Ann Lindstrand. “The immunization Agenda 2030: A vision of global impact, reaching all, grounded in the realities of a changing world.” Vaccine42 (2024): S1-S4.
- Raphiphatthana, Buaphrao, Herdiyan Maulana, Timothy Howarth, Karen Gardner, and Tricia Nagel. “Digital mental health resources for asylum seekers, refugees, and immigrants: protocol for a scoping review.” JMIR research protocols9, no. 8 (2020): e19031.
- Schouten, Barbara C., Antoon Cox, Gözde Duran, Koen Kerremans, Leyla Köseoğlu Banning, Ali Lahdidioui, Maria Van Den Muijsenbergh et al. “Mitigating language and cultural barriers in healthcare communication: Toward a holistic approach.” Patient Education and Counseling103, no. 12 (2020): 2604-2608.
- Truong, Mandy, Yin Paradies, and Naomi Priest. “Interventions to improve cultural competency in healthcare: a systematic review of reviews.” BMC health services research14 (2014): 1-17.
- Uwah, Chijioke, and Priviledge Cheteni. “Revitalizing folklore for HIV/AIDS messaging in South Africa: the impact of theatrical storytelling on public health communication.” Cogent Arts & Humanities11, no. 1 (2024): 2431455.


